Long-term care is variably defined. According to the World Health Organization (WHO), it is “a means to ensure that older people with a significant loss of capacity […] can maintain a functional ability consistent with their basic rights, fundamental freedoms and human dignity” (2015, p. 127). Long-term care can be provided in different places—at home or in a facility—and by different caregivers, including unpaid family members and paid workers.
The WHO recommends that the governance of long-term care begin at the national level, through legislation and coordination. However, “in most countries”, they note, “long-term care falls between different ministries […] this division affects the quality of long-term care services as it can lead to fragmentation and complex arrangements for financing, regulation, information systems and management of services” (2021, p. 12).
In Canada, the long-term care system closely mirrors the WHO’s assessment, as it is fractured by design. Under the Canadian Constitution, provinces and territories are responsible for delivering most health care services—including long-term care—which are funded by provincial or territorial and federal taxes (Government of Canada, 2019). As a result, long-term care is a regional patchwork assemblage, in its administration and delivery. “Jurisdictions offer a different range of services and cost coverage”, notes the Federal Government; “Consequently, there is little consistency across Canada in what facilities are called […] the level or type of care offered and how it is measured; and how facilities are governed or who owns them” (Government of Canada, 2004).
In Ontario, long-term care is further fragmented in its administration and delivery, via services and facilities that include in-home care, retirement homes, and long-term care homes. Long-term care homes in the province—which are the focus of this report—provide “help with most or all daily activities” and “access to 24-hour nursing and personal care” (Ministry of Long-Term Care, 2022). Their scope aligns with the WHO’s description of facilities-based long-term care, which “provide[s] a variety of services, including medical and assistive care, to people who are unable to live independently in the community” (WHO, 2021, p. 54).
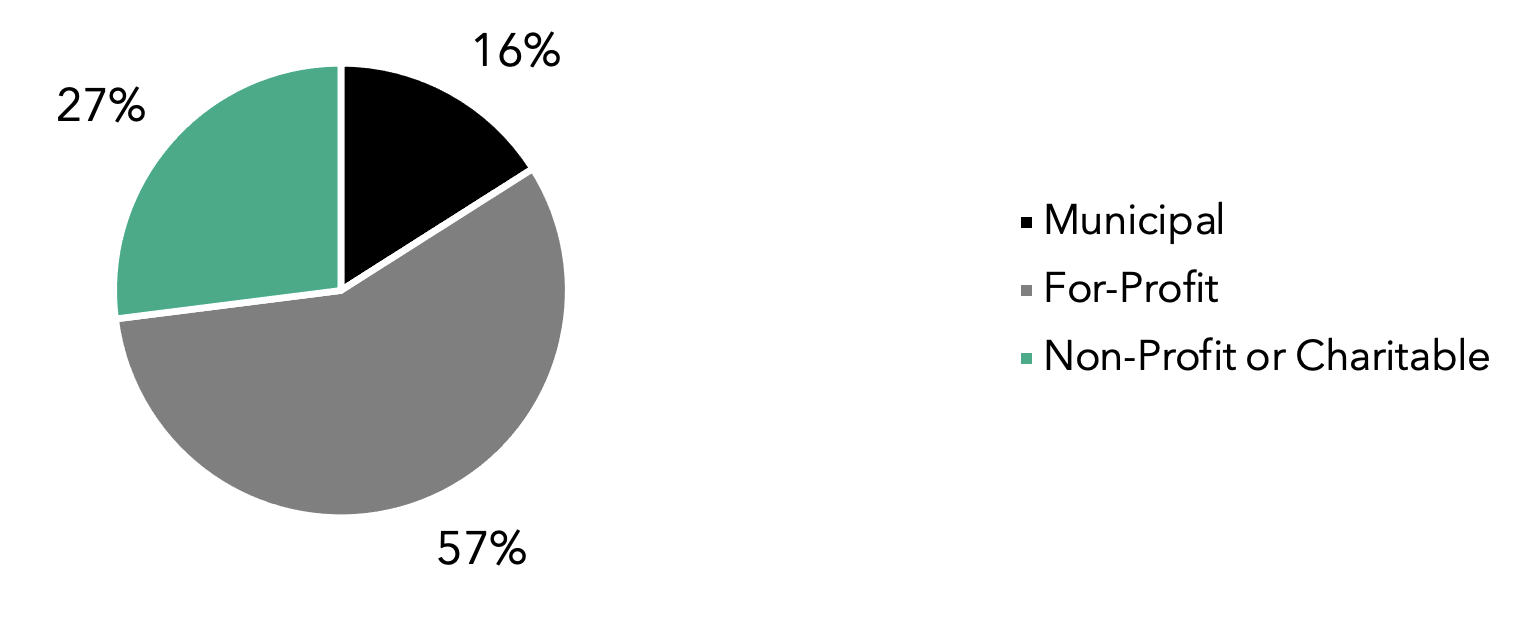
Long-term care homes in Ontario are partially funded by the provincial government, which pays for nursing and personal care, while residents pay for “accommodation charges such as room and board”; the maximum monthly rate for a private room is CAD $2,701.61 (Ministry of Long-Term Care, December 21, 2021). Homes are regulated under the provincial Long-Term Care Homes Act, 2007 and must have a license to operate (Ministry of Long-Term Care, 2022). As dictated by the Act, an administrator “oversees the long-term care home and is responsible for its management”, as the most senior member of staff (Ministry of Long-Term Care, December 20, 2021). Ontario has a total of 627 long-term care homes (Canadian Institute for Health Information (CIHI), 2021a). As shown in Figure 1, licensees include several types of organizations: municipalities (16% of homes), for-profit corporations (57% of homes), and non-profit corporations (27% of homes, including those run by charitable organizations) (Government of Ontario, 2020). Throughout this report, licensees will be referred to as organizations.
Figure 1. Long-term care home types in Ontario (n=627)